An Interview with Janet Benedict, PT, DPT

By Jenna Lindman
In Spring of 2019 I was invited to speak at a luncheon fundraiser for the Elmhurst and Edward Hospital Foundation. It was a lovely event and where I met Janet Benedict, a fellow speaker for the event. Janet was there to talk about the importance of a new program being implemented by her with the support of Elmhurst and Edward hospital to screen cancer patients for physical therapy as a means to improve their health and quality of life. Janet was seated at my table with myself and my family, including my Aunt Carol. My Aunt Carol recognized Janet right away, saying that she was her physical therapist when she broke her leg and that Janet was absolutely wonderful. I wanted to get to know more about Janet and the amazing program she was working on. Janet and I were able to connect several months ago for an interview, I’d like to give her a big thank you for chatting with me and being a warrior for the cancer community!
Would you go ahead and introduce yourself?

My name is Janet Benedict, I am a physical therapist at Elmhurst Memorial Hospital. I have worked there since 1995. I have specialized into lymphedema therapy and become a certified lymphedema therapist. I also went back and got my doctorate degree in physical therapy. Throughout the years I have been working more and more with oncology patients because of the lymphedema diagnosis. Realizing that there are so many other needs a cancer patient may have other than lymphedema and realizing just how underserved that population is. I’ve been working on trying to increase the awareness these rehab oncology patients may have as well as trying to facilitate and place referrals of oncology patients to the rehabilitation program.
Can you explain what Lymphedema is?
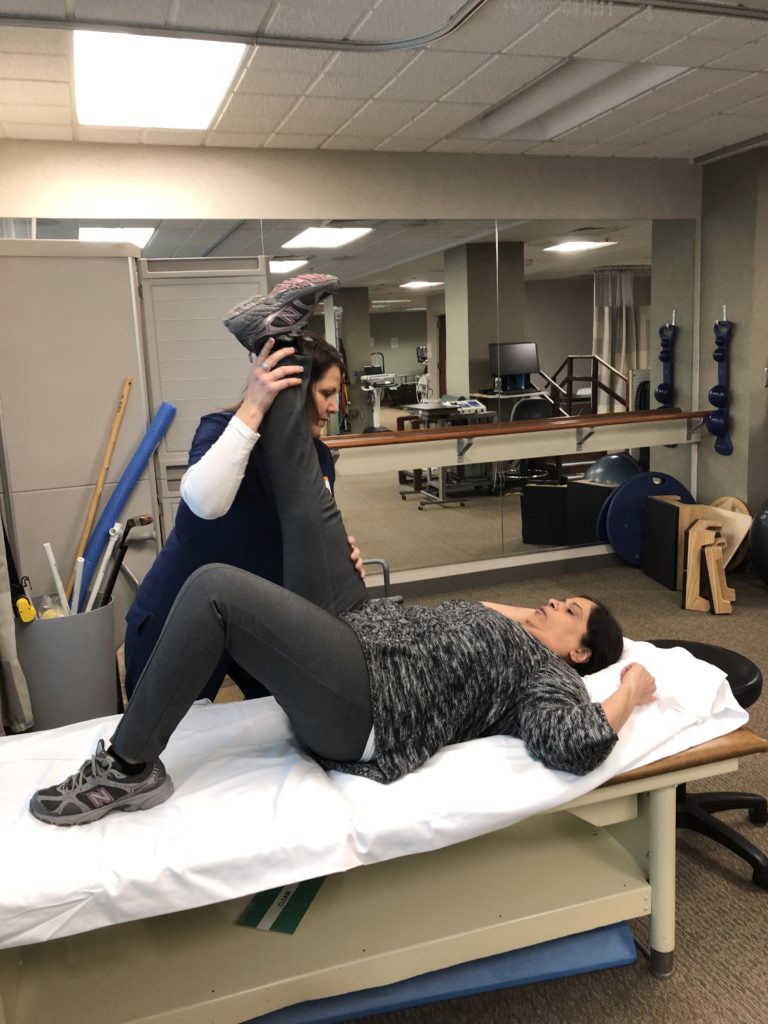
Lymphedema is an abnormality where a patient gets swelling typically in the arm of the leg but can be anywhere: the trunk, the head and neck, the genital areas. In the US the most common cause of lymphedema is due to cancer related treatment; whether it’s the tumor itself blocking the lymphatic system or removing lymph nodes during cancer treatment. This prevents the body from filtering out waste and water causing swelling in those areas. If left untreated the swelling can progress and increase the risk of infection, cause pain, disability, or decrease use of that limb. They can also get nerve entrapment because the swelling is so bad.
So, it’s really important to get lymphedema looked at and treated properly.
Yes, and the earlier the treatment the better. If you recognize the early onset of lymphedema you can treat the symptoms easier. If you wait there can be a big back up of the waste making treatment more difficult to pull the waste. The earlier, the better.
Do you think when people are developing lymphedema, they are aware of what is happening?
It seems that the awareness has been increasing. When I first started treating lymphedema, doctors weren’t referring for it and patients did realize they had it. The thought was, “Oh I have cancer, that’s why I’m swollen.” Patients are now becoming more educated; they are reaching out the to the internet and friends and finding out more about their cancer diagnosis and side effects. Patients are becoming more proactive in talking to their doctors. In addition, doctors are more aware and referring the patient to therapy. Fortunately, Elmhurst Hospital’s oncology practice is proactive in early diagnosis of lymphedema and send the patients to us rather quickly!
Great, I’m so glad you guys have the program. When we first met you talked about prehab for people. What is prehab and how does that work?
Prehab is a common word that you associate with people who would have an orthopedic injury. They would go through therapy prior to having their knee surgery or total hip replacement, things like that. It’s not a common word when you think of the oncology patients – which is too bad because oncology patients have a huge need for rehab services. There is research showing that about 60% of oncology patients have at least one ailment that could be [helped] by rehab. Some research even shows that as high as 90% of oncology patients have something that could be helped by rehab. Unfortunately, about 40% of these patients aren’t bring referred to therapy and depending on what article you read it can go up to 60, 70, 80% of patients that aren’t referred. There’s a lot of discrepancy in the research of the exact numbers, but the common theme is that many oncology patients would benefit from rehab that they aren’t getting. Part of the problem is that insurance is impairment-driven. If you don’t have an impairment for rehab, insurance won’t pay for it. With an oncology patient, the impairment isn’t visible all the time. The main thing on the patient’s mind in their doctor’s appointment is, “What is my outcome?” They don’t necessarily bring up to their doctor that they might be having difficulty walking or need help getting in and out of bed or having difficulty dressing themselves. The doctors can’t visibly see it as well, when they come in the room the patient is already sitting on the exam table. So, it’s an unseen limitation.
What benefits have you seen of rehab?
We see an improvement in quality of life for patients that have been referred to therapy. Some of these side effects patients experience when they have cancer treatment can be weakness and pain, balance impairment, or chemo brain. Because of that, a patient might not be able to go to work or school, they might have trouble getting out of bed, they may not be able to make dinner or care for their families. When you’re not able to do these normal daily activities, it can be depressing. Patients can lose their independence and who they are as a person. By working with them in rehab we can help get their strength and mobility better so they can become the person they were before cancer. Not only is that really empowering for the patient, we are finding that rehab is also very beneficial to the insurance companies and to the hospital. Research is finding that rehab is decreasing length of hospital stay and complications of treatment because the patient is stronger and there are overall less readmission rates to the hospital.
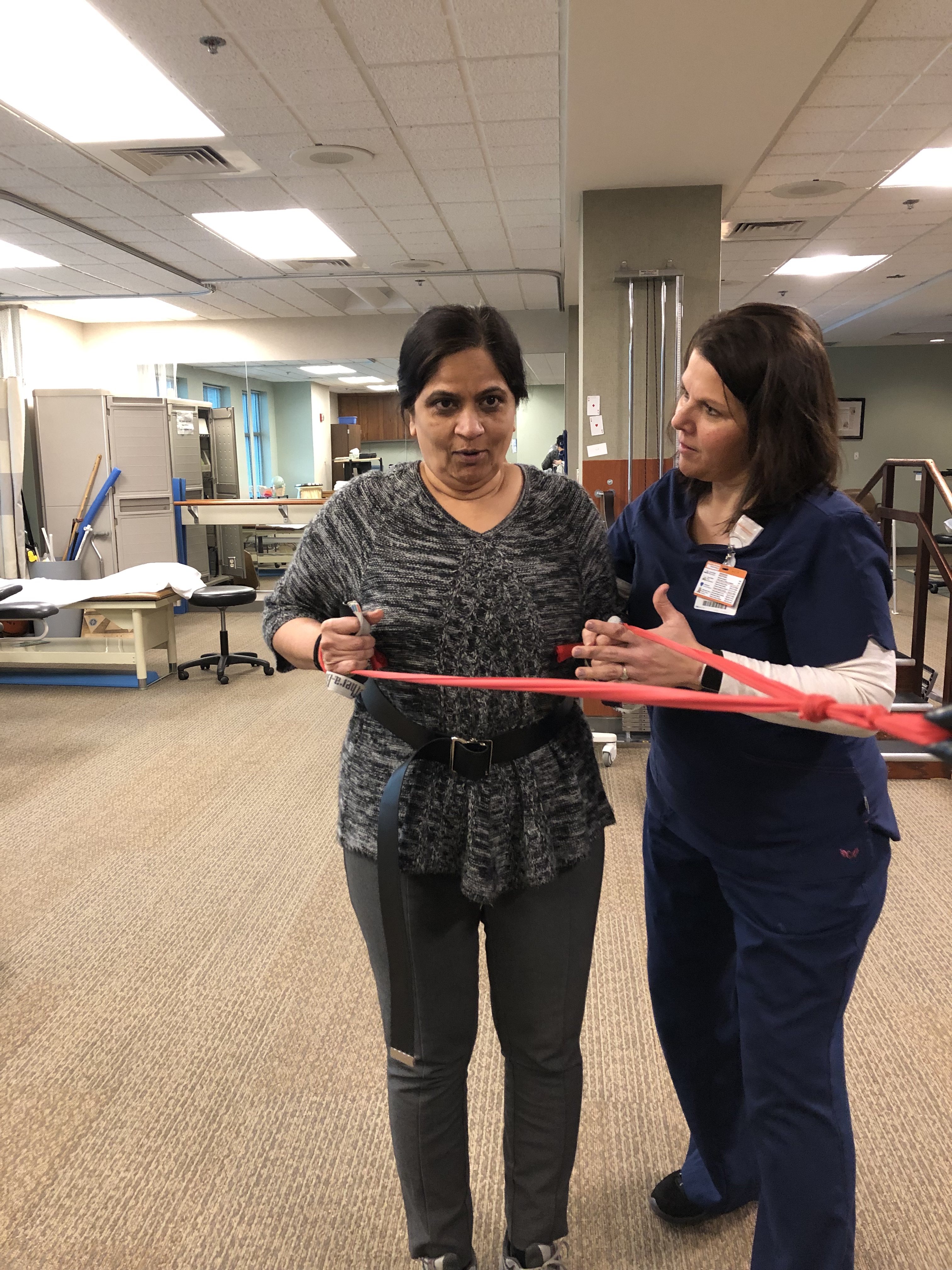
This is all very well researched, but not being well implemented in hospitals across the country. We have started a program at Elmhurst and Edward Hospital called Oncology Screening with the support of Edward and Elmhurst foundation. The Foundation has offered to support these oncology screenings. We are starting with a small number of patients as a pilot to see how the program goes. We selected a few oncology surgeons referring their patients prior to their oncology surgery to screen. It’s free of charge, provided by the foundation. We do an assessment of what their physical mobility to determine if they would benefit from physical therapy or occupational therapy prior to their surgery. If we do determine therapy would be beneficial, the doctor gives the order for rehab and we now have an identifiable impairment that the insurance company will pay for. This is a very new program, we only have a small handful of patients that have participated in it, but the patients have been very appreciative of the services that we offer.

Do you know of any other hospitals try to implement this?
I don’t know of any other hospitals, that doesn’t mean there is not. We started doing these screenings back in 2014 specifically for breast cancer patients that have seen wonderful results and success with which is why we expanded it to the full oncology population. I know of a couple of hospitals that do a similar screening for their breast cancer, but I feel that ours is more in depth and personal for the patient. Ours are also free of charge, other hospitals are billing the insurances. If the insurance denies payment for this service, the patient may be responsible for paying.
As a cancer survivor myself, when it came to rehab I would think, “Well, why would I need that?” But looking back I think that it would have been beneficial for me because of how weak I got, even as a young person. I am wondering if this is something that is beneficial for people of all ages going through cancer?
Absolutely! Like you said you were young and going through it you didn’t realize you had the deficits until you were looking back. When we talk about having a patient come for therapy it doesn’t have to be 12 sessions; sometimes even two or three sessions is enough for a patient to build up the confidence to say, “Oh, I can do that exercise.” They start to do it more on their own and build strength. We work with a wide age range of patients. We don’t look at their age as whether they should have therapy or not, it’s more looking at their function: What was their function prior to being diagnosed with cancer? And what is their function now?
I wonder, what makes you so passionate about this program?
I really don’t know! When I first started working as a physical therapist it was mostly for orthopedic patients. In 2005, the lymphedema therapist we had was moving out of state and our manager was trying to find someone to take some classes in lymphedema classes to be able to see the one or two patients a year we got. I was convinced to go, and I just found it extremely interesting. I started seeing the patients and [after some time] we started seeing several dozen patients a year. That’s when they sent me to become a certified lymphedema therapist so I could treat the more complicated cases. Over the years the program kept growing I was proactive in trying to get early intervention for lymphedema and started I was realizing that lymphedema wasn’t their only need.
The oncology population is a rewarding population to work with. To know that you are helping someone through this difficult period of their life and improve on anything that to get them get through this journey. I’m very thankful to Elmhurst and Edward Foundation because not all insurances will pay for these screenings. Because of the cost, I think that’s why a lot of hospitals aren’t able to do them. Financially, it is a loss for the hospitals. But the Elmhurst and Edward Foundation are so gracious and supportive in what I’m trying to do for this population and realize that this is something that we should be doing.
If you can show the program is beneficial, which I’m sure it’s going to be, is there is a way to present it to the insurance companies to prompt them to pay for these screenings, especially if it’s going to benefit them?
I’m just hoping that more research is published — that’s where the power is really going to be to show the insurance companies the need of it. It is a financially smart way to move forward to decrease costs. But because it’s such an unknown area, it’s not being realized. Hopefully other hospitals will see what Elmhurst and Edwards are doing and start doing it as well. It’s going to take an army to get the insurance companies to change.
Do you have any special stories of someone who received therapy or was grateful for your services?
The oncology population are so appreciative, and I think that’s why I love working with this population so much. I probably get more hugs and thank yous than any other therapist in the department. They truly are so gracious. I have patients that write letters to my manager. It’s amazing how these patients respond to me. I just recently had a patient who came back to say “hi” and say that she was doing well. It was so great to have a patient come to show me how they made it through and how much better they are doing.
It must be truly an amazing program because I think that people are more inclined to complain about something than give a complement. The fact that you have so many people coming back and saying hello shows how impactful it is.
We actually have patients being treated at the University hospitals who have heard of our therapy programs and have asked their doctor for an order to specifically come see us at Elmhurst Hospital.
That’s wonderful! Earlier you spoke about how therapy improves quality of life and how it impacts not just the physical but the emotional. Can you speak a little but on the emotional impact?
When you have a caner diagnosis, a person can go through a wide range of emotions. They can have a level of depression because of the cancer diagnoses and also because they can’t do the things they used to do. People identify themselves with the things that they do; with their work, their family. If you take that away from them, they sort of lose who they are as a person. By having rehab for some of those patients, we are giving their lives back to them. With rehab we get them back to their normal lives.
That’s so important. I’m wondering is there anything else you really want us to know about the program?
Working with the oncology population isn’t just new for the doctors to order therapy for, it’s also new for the therapists to work with oncology patients when they are used to working with orthopedic, stroke, or brain injury patients. It’s a new process and mindset that the therapist must learn to become comfortable working with the patients. Unfortunately, cancer diagnoses have a stigma that because this person is sick, they shouldn’t be doing exercise or going out in public. Much of that stigma is because of the television shows and movies that are out there. When they show a person, who has cancer they are showing them getting violently ill and not being able to move. Many patients aren’t sick during their cancer treatment and are finding that getting back to the activity level they had before cancer can help them tolerate their treatments better. It’s a new mindset that everyone has to adapt, it is okay to work with someone who is having chemotherapy. You just have to be smart about it.
Thank you for talking on that! I remember when I was going through treatment, although there were times when I was very sick, on the days I felt like I could get up and do something I felt like I shouldn’t.
Exactly. It’s a mindset change that the patients, the family members, and therapists must have. Fortunately, the oncologists want you to work and be active and rehab is the key of how they get there.
I wonder if someone is interest in your program or in helping, how can they do so.
Elmhurst and Edward foundation always welcome donations. Anybody interested in helping can contact the Foundation and specifically mention the oncology screenings. This is a program that is just starting out at Elmhurst and Edwards, so if a screening program isn’t available a patient can bring up the physical deficits they are having to their doctor and ask if they can have an order to go to rehab. Rehab also includes occupational therapy which can help with fine motor activities, neuropathy, and adaptive equipment and speech therapy that can help with cognitive deficits in relation to chemo brain, swallowing, talking, memory, to name a few.
I hope we get to the point someday when these screening become regular!
It would be great that eventually, we don’t need these screenings and everyone can be more aware of these physical needs a patient may have.
Is there anything else you’d like us to know?
Just that I love what I do.
And it shows. Thank you so much for letting me interview you, Janet! You are up to amazing things for the cancer community.
If you would like more information on the Elmhurst Memorial and Edward Foundation, please see the links below.



